Abstract
Introduction
Acute lymphoblastic leukemia (ALL) is the most common type of childhood cancer with, an incidence rate of 7.55 cases per 100,000 person-years for males aged 0-4 in the Canadian population. Thromboembolism (TE) is a well-recognized serious complication associated with ALL that results in significant morbidity and occasionally mortality. In patients with ALL, the reported incidence of symptomatic and asymptomatic TE is as high as 16% and 37%, respectively. At diagnosis, there is evidence of increased thrombin generation in children with ALL. Patients often present with a hypercoagulable state and this prothrombotic condition persists during the treatment period, indicating a possible interaction of the disease and therapy. Since the efficacy and safety of thromboprophylaxis during ALL treatment are still being explored, understanding the biology of the disease is crucial for defining the optimal strategy for prevention and management of ALL-associated thrombosis.
In this study, we aim to explore a better understanding of how ALL affects the hemostatic balance. Due to the low incidence of leukemia, single-center studies are not adequately powered to detect significance. This meta-analysis was conducted to comprehensively evaluate the hemostatic profile at the time of diagnosis in pediatric ALL patients.
Method
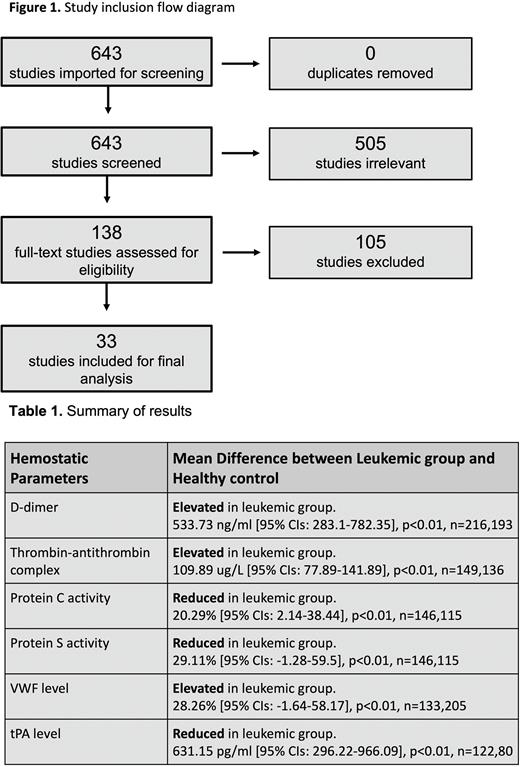
PubMed database was searched on December 2021 with the following keywords: "acute lymphoblastic leukemia", "coagulation", "fibrinolysis" and "hemostatic." The inclusion criteria were: 1) study participants with childhood ALL, 2) hemostatic parameters were measured and reported at the time of diagnosis, 3) there is a comparator group of healthy subjects, and 4) there is no other reported comorbidities. Non-human studies, non-English articles and studies without healthy comparators were excluded. Data on coagulation profile at diagnosis were collected and meta-analyzed. The statistical method was random-effect inverse-variance weighting. The results were reported as mean difference with 95% confidence intervals (CIs)
Result
The initial search yielded 643 articles. Of these, 505 studies were excluded from title/abstract screening. The fulltexts of the remaining studies were screened, and 33 studies were included for the final analysis. D-dimer levels were elevated in the Leukemic group by 533.73 ng/ml [95% CIs: 283.1-782.35], p<0.01, n=216,193. Thrombin-antithrombin complex levels were also increased in the Leukemic group by 109.89 ug/L [95% CIs: 77.89-141.89], p<0.01, n=149,136. In addition, the levels of natural anticoagulants were reduced in the Leukemic group. Protein C activities were lower in the Leukemic group by 20.29% [95% CIs: 2.14-38.44], p<0.01, n=146,115. Protein S activities were lower in the Leukemic group by 29.11% [95% CIs: -1.28-59.5], p<0.01, n=146,115. Furthermore, markers of endothelial dysfunction were elevated in the Leukemic group. VWF levels were increased by 28.26% [95% CIs: -1.64-58.17], p<0.01, n=133,205 while tPA levels were reduced by 631.15 pg/ml [95% CIs: 296.22-966.09], p<0.01, n=122,80.
Significance
Children with ALL already present with hemostatic imbalance at diagnosis, favoring a hypercoagulable state. Interestingly, there has been little research on thrombin markers prior to chemotherapy in childhood ALL. The majority of data were extracted from prospective studies investigating the effect of therapy on thrombosis. Our study highlights significant differences from healthy control levels in D-dimer, Thrombin-antithrombin complex, protein C activity, protein S activity, VWF and tPA levels in children with ALL at diagnosis. Better tools of prediction would allow prospective identification of patients in whom prophylaxis might reduce the risk of thrombosis.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal